What Is The Eustachian Tube?

The Eustachian tube is a small passageway that connects the middle ear to the back of the throat. The Eustachian tube plays a critical role in regulating the pressure within the middle ear, which is necessary for healthy hearing. It also helps to drain any fluid that may accumulate in the middle ear, preventing the growth of bacteria that can cause ear infections. When you swallow, yawn, or chew, the muscles in the back of the throat open the Eustachian tube briefly, allowing air to flow in and out of the middle ear, equalizing pressure. If the Eustachian tube is blocked or not functioning correctly, pressure within the middle ear can build up. This can ultimately lead to ear pain, hearing loss, and other complications.
The eustachian tube is closed at rest in a hearing auditory system. As noted above, it opens when swallowing, yawning, or chewing to equalize pressure in the middle ear space. This maintenance of middle ear pressure is important not only for the health of the tympanic membrane and mucosal lining of the middle ear, but for sound transmission to the inner ear.
What Is Eustachian Tube Dysfunction (ETD)?
An abnormal eustachian tube may present as inadequate opening, or obstructive eustachian tube dysfunction, or a eustachian tube that remains open unnecessarily, or patulous eustachian tube dysfunction. While the two are seemingly opposite disorders, they often present with similar symptoms and complications.
Obstructive Eustachian Tube Dysfunction
This condition implies a Eustachian tube that cannot be opened properly. Common symptoms include:
• Ear pain
• A feeling of pressure or fullness in the ear
• Hearing loss
When the eustachian tube can’t open properly, it can result in a build-up of pressure and/or fluid. This can result in otitis media, ear drum retraction, and even more significant disorders like cholesteatoma if left untreated. Obstructive ETD can be caused by a myriad of things such as allergies, sinusitis, and even a simple common cold.
Patulous Eustachian Tube Dysfunction
This condition is a disorder that causes the Eustachian tube to remain open. Common Symptoms Include:
• Ear pain
• Pressure or fullness
• Aerophony (when patients hear their own breathing)
• Autophony (when the patient’s own voice sounds abnormally loud, low pitch, or reverberant)
There is significant overlap in the symptoms associated with patulous ETD and obstructive ETD and patients can even present with a combination of the two disorders further complicating ETD diagnosis. Causes of patulous ETD vary from that of obstructive ETD, however, and include significant weight loss, allergies, radiation therapy, acid reflux, pregnancy, and even stress. While this is often a temporary problem with no long term risks or effects, the symptoms cause by patulous ETD can certainly affect a patient’s quality of life
Eustachian Tube Function Test: How to Diagnose Eustachian Tube Dysfunctio
While tympanometry can indirectly assess eustachian tube function, it’s sensitivity to dysfunction is limited. At times a negative middle ear pressure is indicative of eustachian tube dysfunction, however, individuals can also have ETD with normal middle ear pressure.
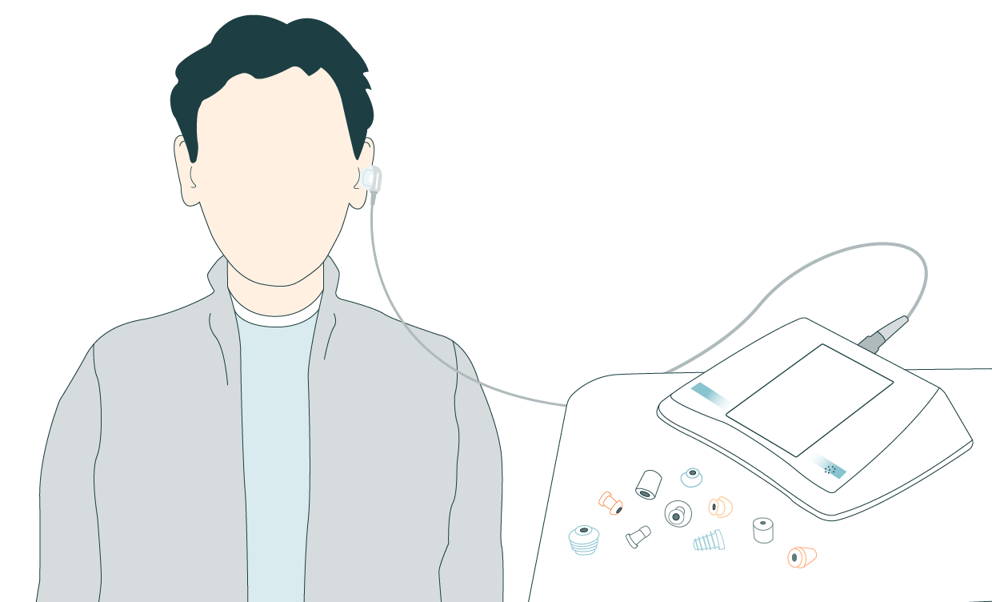
There are two main assessments of eustachian tube testing; one detects blocked or abnormal eustachian tube function and the other detects a patulous eustachian tube. Like tympanometry, eustachian tube testing is quick and non-invasive.
Testing for Eustachian Tube Dysfunction
Many clinicians utilize traditional tympanometry to assess eustachian tube function. During the test, a probe is placed in the ear and air pressure is fluctuated as the movement of the tympanic membrane is measured 3 times. The first tympanogram is completed normally. The patient is asked to swallow or take a sip of water and then the second measure is completed. The patient is then asked to swallow a second time and the final measurement is performed. During this final measure, a clinician may ask the patient to perform the Valsalva maneuver in place of a second swallow. The Valsalva maneuver is a method used to open the eustachian tube by pinching the nose and blowing out with the mouth closed. When the eustachian tube is functioning normally, the peak pressure of each of these three tympanogram should shift with a difference of 15 – 20 daPa between each of the measures.This is because the actions performed by the patient, swallowing or drinking water, are causing the eustachian tube to open and close.
With eustachian tube dysfunction, the three tympanograms will have similar peak pressures, meaning the eustachian tube is not functioning normally.
A Patulous Eustachian Tube Test Method
In tests looking for patulous eustachian tube, eustachian tube closure is assessed by looking for tympanic membrane movement that occurs synchronously with breathing. While some clinicians monitor this visually, with microscopic otoscopy, it is possible to measure this more quantitatively through continuous impedance measures.
Like tests of eustachian tube measures described above, a probe is placed in the ear like during traditional tympanometry. A probe tone is introduced and acoustic immittance is measured. While the patient is asked to breathe first normal, then deeply, and finally they are asked to hold their breath for a short period of time. With a non-patulous eustachian tube, tracings will appear random and not in-sync with breathing rhythms. If a patulous eustachian tube is present, tracings will follow for the pattern of breathing.
It's important to note that this method is only sensitive to patulous eustachian tube while the patient is symptomatic and cannot detect intermittent patulous eustachian tube. As such, it is important to consider patient history and symptoms in your diagnosis.
Why You Should Test Eustachian Tube Functionality
At times, patients can present with the aforementioned symptoms, but with normal tympanometry and audiometry. Without testing eustachian tube function, these patients can go undiagnosed and risk a decline in quality of life and the development of other ear disorders like otitis media and cholesteatomas.
If detected early, simple treatments like avoiding allergens or taking over the counter (OTC) antihistamines and decongestants can alleviate symptoms. Severe eustachian tube dysfunction in rare cases can require surgery. Thus, it is important to follow up with your doctor if the aforementioned conservative treatments are ineffective.
Additionally, eustachian tube function can be tested prior to other middle ear surgeries, like tympanoplasty to monitor symptoms and predict operative success. For example, it has been noted that a successful tympanoplasty is more likely in patients with normal eustachian tube function than those whose ETD persists post-operatively.
The Eustachian tube's proper functionality is crucial for maintaining healthy hearing. Testing the Eustachian tube's function is necessary to diagnose patients with middle ear related complaints accurately. Additionally, with eustachian tube testing a complete and appropriate treatment plan can be set in motion.
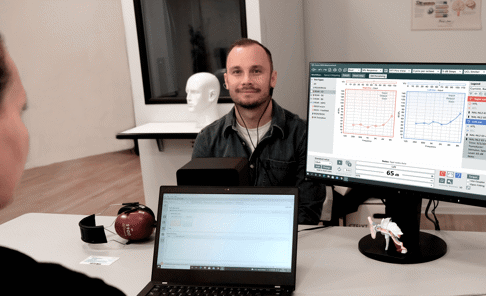
Auditdata Measure - Tympanometry
Test The Functionality Of the Eustachian Tube With Measure
When it comes to testing the functionality of the Eustachian tube, it's important to have an efficient and user-friendly tympanometer. The Measure Tympanometer is an ideal choice for clinicians, offering battery operation, reliability, and user-friendly interface. With a touch screen and streamlined interface, you can easily perform multiple tympanometric measures in succession, making the testing process quick and efficient.

Other Blogs You Might Enjoy:

The History of Audiometry and The Evolution of Audiometers
In short, audiometry is the study of the sensitivity of an individual’s hearing that has been performed for more than 150 years! An audiometer is a tool used to ascertain this information. This blog elaborates on the history of audiometry, and the evolution of audiometers as these are closely intertwined with not only each other but the advancement of the field of audiology as a whole.
Are Real Ear Measurements Necessary?
Real Ear Measurements (REM) – also called Probe Microphone Measurements (PMM) – are considered the gold standard in hearing aid fitting and verification, allowing audiologists to determine whether a hearing aid user is receiving the precise level of amplification needed at every frequency to maximize their hearing. This blog explains how REM can improve customers’ hearing, as well as drive better business outcomes and serve as a key differentiator for hearing clinics.

Cochlear Dead Regions: How To Assess With TEN Testing And Manage With Frequency Lowering
Hearing loss is a common problem, affecting millions of people worldwide. It can be caused by a variety of factors, including age, noise exposure, genetics, and illness. In some cases, individuals with hearing loss may experience cochlear dead regions, which can make it difficult to understand speech and other sounds. In this article, we will discuss cochlear dead regions, how to identify them with TEN testing, and managing dead regions with frequency lowering in hearing aids.
Don't Miss Out On the Latest Insights On Audiology
Sign up today to receive exciting updates, tips, and the latest newsletters from Auditdata.