What are Otoacoustic Emissions
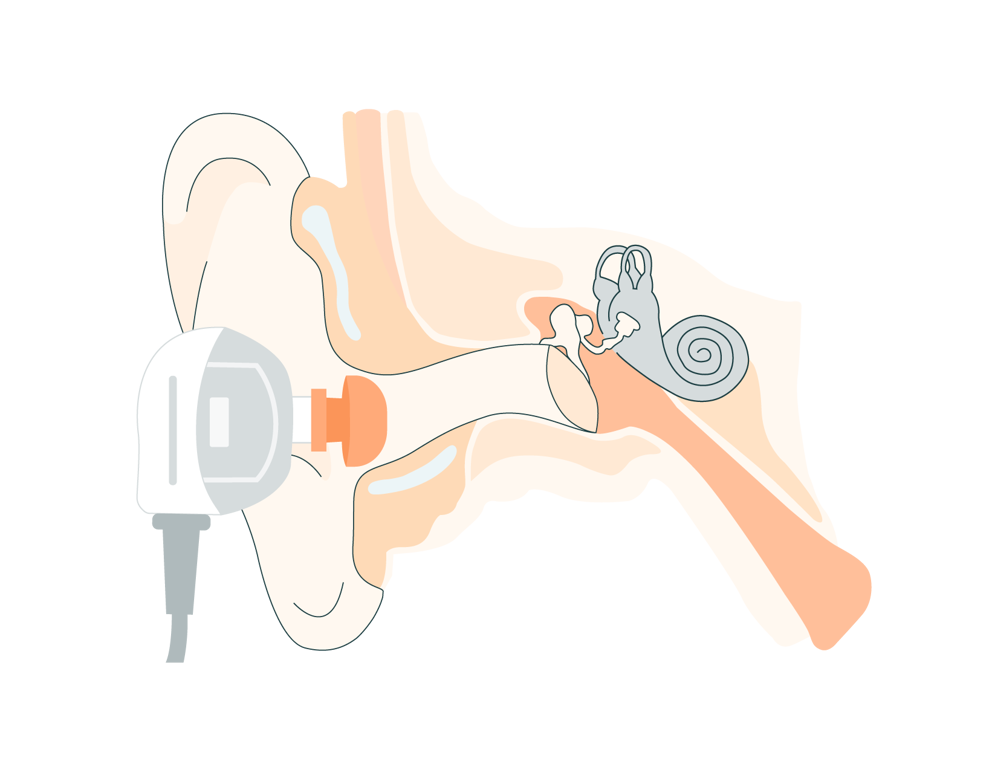
Otoacoustic Emissions are sounds generated by the cochlea in response to auditory stimuli. When sound enters the ear, hair cells within the cochlea vibrate, producing these emissions or sounds. The emissions are then transmitted across the middle ear to the external ear canal, where they can be recorded. Thus, a healthy middle and outer ear is needed to detect these faint responses.
What OAE Testing Is and Its Importance in Audiology

The OAE test plays a crucial role in various audiological evaluations. It is commonly used in newborn hearing screenings to detect hearing loss early, ensuring timely intervention and support. It is also valuable for monitoring hearing health over time, especially for individuals at risk of noise-induced hearing damage or ototoxicity. The OAE test measures these emissions using a sensitive microphone placed in the ear canal. By analyzing the presence or absence of OAEs, audiologists can assess the integrity of the cochlear function.
OAE testing stands as a cornerstone in audiological practice, offering a non-invasive and objective means of assessing cochlear function. From newborn screenings to differential diagnosis and monitoring hearing health, its importance in preserving and enhancing auditory function cannot be overstated. As technology advances and research progresses, OAE testing continues to evolve, reaffirming its indispensable role in the field of audiology and the broader pursuit of hearing health and well-being.
Types of Otoacoustic Emissions
-
Spontaneous otoacoustic emissions (SOAE) are sounds produced by the ear without any external sound source, and they can be detected using microphones inserted into the external ear canal. These emissions typically range in frequency from 500 Hz to 4,500 Hz.
-
Evoked OAE (EOAE), require an acoustic stimulus prior to their measurement or emission. There are three types of EOAEs: transient evoked, stimulus-frequency, and distortion product OAEs. Transient evoked and distortion product OAEs are the two most used clinically.
-
Transient-evoked OAE (TEOAE) are elicited using either a click or tone-burst stimuli. A click stimulus possesses a sudden onset, brief duration, and spans a wide frequency range up to 4 kHz, aiming to evoke responses from multiple nerve fibers. In contrast, tone burst stimuli are delivered within a narrower frequency range, especially at lower frequencies, to elicit more frequency-specific responses.
Detecting a response when testing TEOAEs can be difficult as the response emission mirrors the stimulus frequency. Thus, multiple stimuli and responses are elicited and averaged to distinguish the emission from the stimulus. Response emissions exhibit latency periods ranging from 2 to 23 milliseconds, corresponding to the frequency of the stimulus. Higher frequencies, which travel shorter distances along the basilar membrane to the base, exhibit shorter latencies, while lower frequencies, traveling further towards the cochlear apex, require longer latencies.
-
Stimulus-frequency OAEs (SFOAEs) are evoked using pure tone stimuli. Like TEOAEs, the response emission is the same frequency as the stimulus, making responses difficult to distinguish. As a result, this type of OAE is rarely used clinically.
-
Distortion-product OAE (DPOAEs) are elicited by employing two concurrent pure tone stimuli (f1 and f2). The main test frequency is referred to as f2 whereas f1 is determined by a fixed ratio in reference to f2.
In contrast to TEOAE, which offers a comprehensive assessment of cochlear function across a wide frequency spectrum, DPOAE can be tailored to evaluate frequencies aligned with the patient’s audiogram, thereby enhancing sensitivity in detecting high-frequency hearing impairments.
When measuring the DPOAE, the largest response emission should occur at the frequency calculated from the formula: 2f1-f2. This makes DPOAEs easily distinguishable from the presented stimuli as the resulting frequency is different from the two presented stimuli. Typically, DPOAEs are recorded at 1-6k Hz, but they can be elicited at frequencies as high as 10-12k Hz depending on the equipment used.
Decoding the OAE Test: Fundamentals and Significance
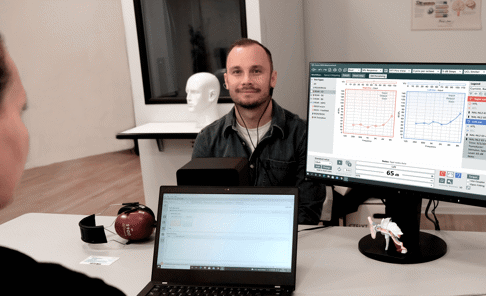
Executing OAE Testing: Procedures and Best Practices
A thorough understanding of the preparation and procedural steps involved in Otoacoustic Emissions (OAE) testing is essential to ensure accurate and reliable results. When performing OAE testing, it’s important to consider:
Preparation
- Make sure the patient’s ear canal is clear of debris or obstructions through
- Perform tympanometry before the OAE test whenever possible. Note any middle ear dysfunction as this can influence OAE results.
- Conduct the test in a quiet environment to minimize external noise interference. Sound-treated booths or rooms are ideal for optimal testing conditions.
- Position the patient comfortably, ensuring a snug fit of the probe in the ear canal. Stable positioning reduces artifact and improves the accuracy of measurements.
- Regular calibration of OAE equipment is vital to maintain accurate and consistent test results. Calibration of OAE equipment should occur annually. In addition, hearing healthcare providers should perform daily checks of OAE equipment through real-ear tests or probe integrity tests. Follow manufacturer guidelines for calibration procedures.
After the test
- Interpret OAE results in conjunction with patient history, clinical observations, and other diagnostic tests. Consider age-specific norms and other factors, like artifact, that may influence OAE responses.
Record detailed information about the test procedure, including equipment used, patient demographics, test parameters, and results
Clinical Applications of an OAE Hearing Test
The OAE test extends beyond basic hearing screenings, finding utility across diverse clinical scenarios. Firstly, it serves as a valuable tool for monitoring cochlear function in patients undergoing ototoxic medication regimens, aiding in the early detection of potential auditory damage. Additionally, the OAE test plays a crucial role in differentiating between cochlear and retrocochlear pathologies in individuals with auditory processing disorders, facilitating targeted treatment strategies. Furthermore, it proves beneficial in assessing auditory function in individuals with developmental disabilities who may encounter challenges in participating in traditional behavioral hearing tests, offering an alternative means of evaluating their hearing capabilities. Through its versatility, the OAE test enhances diagnostic precision and contributes to more tailored interventions for patients across various clinical contexts.
OAE testing holds significant importance in audiology for several reasons. Firstly, it facilitates early detection of hearing loss, crucial in newborn screenings, allowing for timely interventions critical for language and cognitive development. OAE testing can also be used to monitor hearing health over time, especially in individuals at risk of noise-induced hearing damage or ototoxicity, enabling timely interventions to prevent further loss.
OAE testing provides an objective measure of auditory function, particularly advantageous in assessing hearing in infants, young children, and individuals with communication or cognitive impairments. Furthermore, it contributes to ongoing research in audiology, enhancing our understanding of auditory physiology and pathology, while also finding applications in specialized areas such as auditory processing disorder evaluations and monitoring cochlear function in patients undergoing ototoxic medication regimens.
Role in Early Detection and Ear Health Screening
-
NIHL occurs due to prolonged exposure to loud noises, resulting in damage to the hair cells in the inner ear. OAEs are sounds generated by the cochlea in response to external stimuli, such as sound. In individuals with healthy hearing, OAEs are typically present, indicating normal cochlear function. However, in cases of NIHL, where there is damage to the cochlear hair cells, OAEs may be diminished or absent. This damage may precede hearing loss that can be detected with pure tone audiometry. Therefore, OAE testing can aid in the early detection and monitoring of NIHL by assessing the integrity of the cochlear function. This information is crucial for implementing preventive measures and interventions to mitigate further hearing loss in individuals exposed to hazardous noise levels.
-
Ototoxic drugs, like certain antibiotics and chemotherapy agents, primarily affect the outer hair cells and can be detected through OAE testing before abnormalities appear on a traditional audiogram. OAE testing offers rapid application and cost-effectiveness, making it a practical choice for monitoring patients throughout their treatment journey. Distortion-product OAEs (DPOAEs) are particularly sensitive to changes in higher frequencies, which are often the first to be affected by ototoxicity. Before initiating ototoxic medications, patients typically undergo baseline OAE testing, with subsequent tests conducted after each dose. A decrease of 2.4 dB or more in OAE amplitude is considered significant, indicating a change in cochlear function and prompting further evaluation.
-
Newborn hearing screening has become a routine practice in hospitals across the country, serving as the standard of care. Its primary goal is to identify newborns who may have hearing impairments and thus need further assessment. Additionally, it aims to detect infants with medical conditions that might lead to delayed onset hearing loss, enabling the development of ongoing monitoring strategies for their hearing health.
Otoacoustic emissions (OAE) are often used for newborn hearing screenings due to their efficiency and reliability in detecting potential hearing impairments shortly after birth. OAE testing is non-invasive, quick, and can be performed while the infant sleeps, making it particularly suitable for screening newborns. Additionally, OAEs provide objective measures of cochlear function, allowing for early identification of hearing loss even before infants can respond to sound through behavioral testing. This early detection facilitates timely intervention and support, crucial for ensuring optimal language and cognitive development in newborns.
-
As OAE tests measure the peripheral auditory system, retrocochlear issues typically manifest with normal OAE results alongside abnormal audiograms and auditory brainstem responses (ABR). Auditory neuropathy spectrum disorder (ANSD) is a retrocochlear disorder often diagnosed and monitored with OAE testing. ANSD often presents with abnormal or absent ABR, poor word recognition, and absent stapedial reflexes. However, OAE may be absent if retrocochlear masses compress the internal auditory artery, impeding blood flow to the cochlea. Additionally, OAE might diminish over time in ANSD patients.
Limitations of Otoacoustic Emissions
OAE screening has limitations primarily related to its lack of specificity. False positives can occur due to contamination from external sounds in the testing environment or internal sounds like breathing and swallowing, posing a risk to accuracy. Distinguishing OAE from background noise during analysis can also be challenging, necessitating examination of reproducible data and the signal-to-noise ratio of the OAE waveform.
As OAEs travel through the middle ear, they can be influenced by middle ear conditions such as middle ear effusion, leading to inaccuracies in measurement. For instance, in children with adhesive otitis, despite healthy outer hair cells (OHCs), OAEs may not be detectable. As a result, OAE screening is unable to differentiate between conductive hearing loss and sensorineural loss.
It's also important to note that OAEs do not directly assess hearing ability or determine the type or severity of hearing loss, unlike pure tone audiometry. However, they play a vital role in both newborn hearing screening and diagnostic audiology, aiding in the identification and differentiation of various hearing conditions.
Screening vs Diagnostic OAE tests
Screening OAE tests
Just like pure tone screenings, the goal of screening OAEs is to differentiate individuals at risk for an auditory disorder from those not at risk of an auditory disorder. During OAE screenings, a pass or refer results is obtained. Test protocols are dependent on equipment, but usually require the detection of emissions in 3 of 4 tested frequency bands for a passing result. When a pass is obtained, there is a low chance of auditory disfunction. It is possible, however, to obtain a passing result with mild hearing loss. TEOAEs may be present for hearing loss in the 25 – 35 dB HL range and DPOAEs may be present for hearing loss in the 25 – 40 dB HL range. When a pass is obtained, but auditory disfunction is present, this is called a false negative. False negative results, while possible, are rare.
A refer result can mean a hearing loss or other auditory disorder is present, it can, however, also occur due to incorrect testing techniques or artifact. When a refer occurs in the absence of an auditory disorder, this is called a false positive.
Diagnostic OAE tests
Diagnostic OAE measurements offer invaluable insights into various conditions, including cases where behavioral testing is challenging, non-organic hearing loss (malingering), noise-induced hearing loss, auditory neuropathy spectrum disorder (ANSD), and distinguishing between cochlear and retrocochlear disorders (site of lesion determination). Additionally, they provide information on the effects of ototoxic medications.
It's important to note that in diagnostic OAE testing, results should not be simply categorized as pass or refer. Moreover, protocols suitable for screening newborns may not be appropriate for testing older children or adults.
Comparative Analysis: OAEs vs. Conventional Hearing Tests

One of the key differences between OAEs and conventional hearing tests lies in their underlying mechanisms and the information they provide. OAEs primarily assess the function of the peripheral auditory system, specifically the outer hair cells in the cochlea. In contrast, conventional hearing tests evaluate the entire auditory pathway, including the peripheral and central auditory systems. While OAEs excel in detecting cochlear pathology and providing early identification of hearing loss, conventional tests offer comprehensive information about the type, degree, and configuration of hearing loss, as well as the integrity of the auditory pathway.
Both OAEs and conventional hearing tests have distinct applications in clinical practice. OAEs are particularly useful in newborn hearing screening, monitoring ototoxicity, and assessing cochlear function in difficult-to-test populations. Conventional tests, on the other hand, are essential for diagnosing the type and degree of hearing loss, differentiating between conductive and sensorineural components, and assessing auditory processing abilities.
Frequently Asked Questions
-
Assessing the accuracy of hearing tests depends on various factors including the specific test utilized, the population being tested, and the methodology employed. According to a study published in the Journal of the American Academy of Audiology, distortion product otoacoustic emissions (DPOAEs) have been found to be highly accurate in detecting cochlear dysfunction, with reported sensitivities ranging from 70% to 100% and specificities ranging from 80% to 100%. For TEOAEs, when used in newborn hearing screening, a 66.7% sensitivity and 98.8% specificity has been noted.
However, it's important to note that the accuracy of these tests may vary depending on factors such as the experience of the clinician administering the test, the age and cognitive abilities of the patient, and the presence of comorbid conditions. Therefore, while OAEs are generally considered accurate diagnostic tools, interpreting their results within the context of the individual patient's clinical presentation is essential for ensuring accurate diagnosis and appropriate management.
-
Reading otoacoustic emissions (OAE) test results involves interpreting the presence or absence of emissions and assessing their amplitude and reproducibility. When analyzing OAEs, audiologists typically look for a clear presence of emissions in response to stimuli presented to the ear. Absence of emissions may indicate cochlear dysfunction or hearing loss. Additionally, the amplitude of the emissions provides information about cochlear function, with higher amplitudes generally associated with healthier cochlear function. Reproducibility of emissions across multiple presentations of the stimulus is also crucial, as it ensures reliability of the results. Interpretation of OAE test results should be done in conjunction with patient history, clinical observations, and other diagnostic tests to provide a comprehensive assessment of hearing function.
Auditdata Measure - Tympanometer
Equipment for Otoacoustic Emissions Tests
The Entomed TY-101 is a portable, battery-operated diagnostic tympanometer that offers a variety of advanced features, including DPOAE/TEOAE, FMDPOAE® pressurized OAEs tympanometry, acoustic reflex decay, and more.

Other Blogs You Might Enjoy:

Comprehensive Hearing Test vs. Hearing Screening: Understanding Results, Implications, and Limitations
Explore the role of a comprehensive hearing test as compared to a quick screening. How accurate are hearing tests, and what kind of results can we expect?
Are Real Ear Measurements Necessary?
Real Ear Measurements (REM) – also called Probe Microphone Measurements (PMM) – are considered the gold standard in hearing aid fitting and verification, allowing audiologists to determine whether a hearing aid user is receiving the precise level of amplification needed at every frequency to maximize their hearing. This blog explains how REM can improve customers’ hearing, as well as drive better business outcomes and serve as a key differentiator for hearing clinics.

Common Audiometry and Hearing Loss Myths
Hearing loss is a prevalent condition that can significantly impact an individual's quality of life, yet misconceptions surrounding audiometry tests and hearing loss persist. This article aims to debunk common myths, providing clarity on the audiometric process and the nature of hearing impairment. By dispelling these misconceptions, we can foster a more informed and understanding approach to hearing health.
Don't Miss Out On the Latest Insights On Audiology
Sign up today to receive exciting updates, tips, and the latest newsletters from Auditdata.